Emergency, Law & Health Professions
Gain skills and knowledge that allow for your growth as an individual learner and place you on the path toward your future.
CARE. SKILL. SERVICE.
Online Options
Advanced EMT

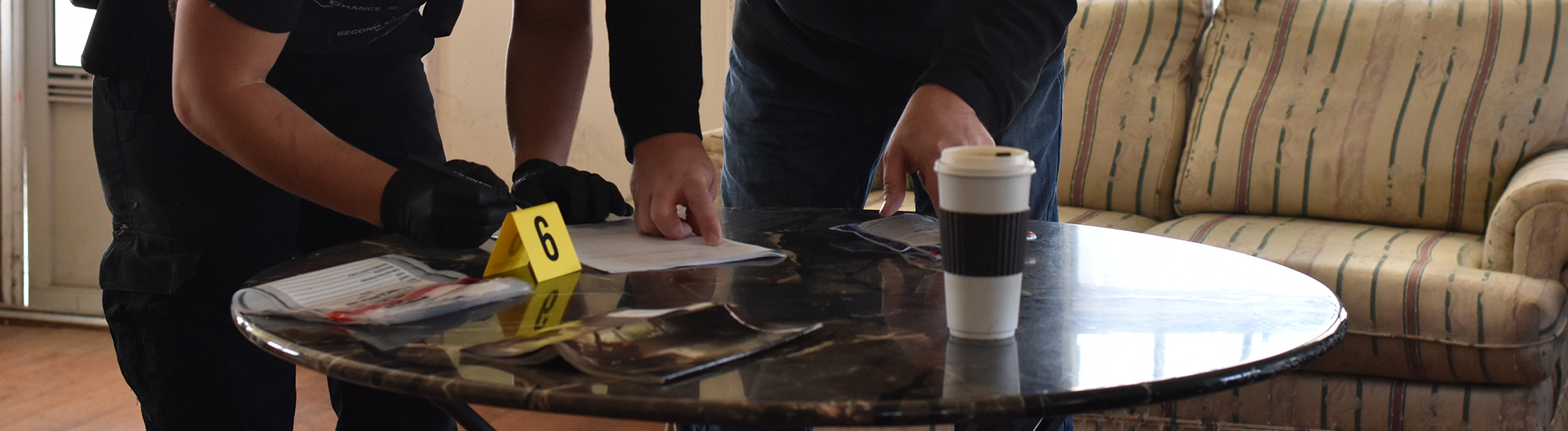
Criminal Justice

Emergency Medical Technician

Fire Science

Healthcare Aides & Assistants

Law (Pre) Transfer

Medical Coding

Medical Office Support

Medical/Health Professions Transfer

MICT - Paramedic

Sonography (Pre) Transfer

Not Sure? Let Us Help
Find our Campus
Location
125 S. 2nd St.
Arkansas City, KS
Contact Info
800-593-2222
admissions@cowley.edu
Take A Tour
Want to take a closer look? Don’t have time to make the trip?
Our Virtual Tour is the next best thing. Follow us for an in-depth look at our beautiful
campuses.
More Areas of Study
Don’t stop now. Dare to move forward with Cowley Online. Get an affordable college education, plus the convenience of online courses.
Cowley College now offers a new agriculture program at our Sumner Campus in Wellington, Kansas. Our program uses an interactive, hands-on approach that takes students from the concept of an idea to the point it reaches the consumer. The Sumner Campus is a new campus that will continue to grow for years.
In two years or less, you can earn certificates for legal, business, & medical offices careers. While our classes teach you how to be successful in your personal and professional life. Learn through experiences by selflessly giving your time & talents to help the community and devote yourself to your education.
Learn how to provide acute care for the critically ill and injured on scene and during transport. Earn credentials for a successful career in law enforcement and corrections. Study these programs prepare students to provide services to communities and individuals.
Enrich your knowledge and skills through diverse writing and literature courses. Contribute to the voice of the students through a newspaper published online and on paper. Perfect skills in photography, broadcasting, news reporting, graphic design and public relations.
Cowley College offers over 120 different programs of study that guides a student on a pathway toward earning a degree or college certificate.







